Sarcomas: New Hope for Overcoming An Aggressive Cancer
When conventional treatments have failed against a particular cancer, or when there are no standard treatment options to ensure survival, many people look for innovative treatments with the hope of extending life. This is often the case when faced with a diagnosis of sarcoma, a relatively uncommon group of cancers that appear to be increasing worldwide, especially among younger people.
Sarcomas are cancers that affect the connective tissues of the body. Connective tissues make up most of the “packing and padding” of the body, the tissues that fill in spaces between other tissues and form the wrappings around organs and other structures. These tissues mainly include fat as well as fibrous tissue surrounding the blood vessels and nerves, tendons, muscle, and bone.
Whereas malignant tumors of the soft tissues are called soft-tissue sarcomas, those that spring up in the bone are called osteosarcomas. Recently, the global incidence of both bone and soft-tissue sarcomas has been on the rise. These tumors are extremely malignant, with a high rate of metastasis, a poor prognosis and a deadly track record overall.
Though surgery can be effective against early-stage sarcomas, the majority of cases cannot be treated with surgery alone because the cancer has infiltrated normal tissues. Prior to 1980, bone and soft-tissue malignant sarcomas of the extremities—mostly in the feet or lower legs—were treated almost exclusively by amputation. Patients who did not want to lose a limb were subjected to extensive surgery around the tumor site, but this often resulted in a very high rate of recurrence.
For these reasons, chemotherapy and radiotherapy became the main treatments for aggressive sarcomas and for preventing recurrences after surgery. Unfortunately, many sarcoma cases are highly resistant to both radiotherapy and chemotherapy. The main goal of both treatments is simply to minimize suffering caused by the disease itself, hopefully extending life in the process. Given the strongly toxic side effects of the treatments, however, the tradeoff can often seem challenging. This is why more effective and less toxic treatments are urgently needed.
Light-Based Treatment Options
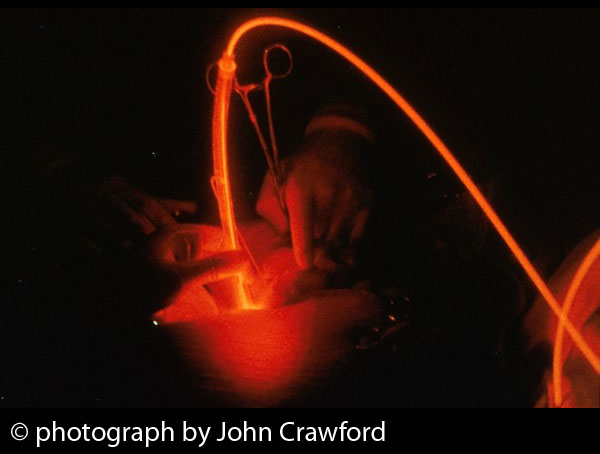
Among the more humane and innovative treatment options that has been considered for sarcomas is photodynamic therapy (PDT). This entails the use of a drug called a photosensitizer, which is activated by a particular type and intensity of light. The best photosensitizers are those that concentrate very strongly in cancer cells as opposed to normal, healthy cells. When photosensitizers are exposed to a specific wavelength of light in the presence of oxygen, they generate a highly reactive form of oxygen that kills malignant cells.
A number of factors can determine the therapeutic success of PDT for people diagnosed with sarcomas. The first consideration is the type of photosensitizer and the type of light that best activates that light-sensitizing agent. (In previous Discoveries articles, we have spotlighted the therapeutic promise of the photosensitizing agent called Bremachlorin®.)
Also, some types of light are able to travel through various tissues better than others. Some, such as lasers, are more focused and penetrating, while others, such as the xenon lamp, can treat a wider area. For these reasons, the choice of an optimal combination of photosensitizer, light source and specific treatment parameters are all crucial to the treatment’s success.
In the past decade, PDT has become an increasingly attractive treatment for sarcomas. Experimental studies have shown that PDT may offer a novel way to treat malignancies such as osteosarcoma, chondrosarcoma, synovial sarcoma, and Ewing’s sarcoma of the soft tissues. Recent clinical research indicates that PDT is an effective treatment for musculoskeletal sarcoma patients, achieving a very low recurrence rate and offering an excellent quality of life, as reported in the October 2014 issue of Oncology Letters.
New Insights from Veterinary Medicine
Scientists in Japan recently developed a novel cancer therapy that combines PDT with hyperthermia, a type of cancer treatment in which body tissues are exposed to high temperatures. In a recent experiment, hyperthermia was shown to synergistically increase PDT’s therapeutic potential against osteosarcoma. The approach can also be combined with local chemotherapy to create a three-pronged strategy that has been called photodynamic hyperthermal chemotherapy, or PHCT.
In this study, the animals were treated at either of two major animal clinics in Japan: Aino Animal Hospital in Shizuoka, or Tokyo Animal Medical Center in Tokyo. The researchers sought to test PHCT against malignant soft-tissue sarcomas in 10 dogs and six cats. In 15 of the cases, surgical treatment was attempted but considered to be insufficient. In one additional case, PHCT was administered without any surgery. The treatment was performed over an interval of one to two weeks and was repeated up to 21 times.
Three chemotherapy drugs were considered as additions to the photosensitizer solution. The main choices were small doses of either bleomycin or carboplatin; for a few cases, a small volume of paclitaxel (brand name, Taxol) was added to the solution. No severe side effects were observed in any of the animals. Treatment was continued for at least three months following surgery. At that point, the researchers only continued the treatment if the animal’s owner requested it. For the second and all subsequent rounds of PHCT, the treatments were carried out with all animals being under sedation.
No disease recurrence was observed in 70% of the dogs and 50% of the cats for observation periods ranging from 238 to 1901 days. These findings may indicate that PHCT decreases the risk of recurrence for soft-tissue sarcomas. Because all of the surgical attempts in these animals had fallen short, a much higher rate of recurrences would have been expected with surgery alone. When the surgical margin is unclear or insufficient—that is, more cancer exists around the periphery that cannot be removed—the recurrence rate for soft-tissue sarcoma is 10 times higher than when the surgical margin is clear or sufficient.
As a post-surgery alternative to radiotherapy, the PHCT strategy combines PDT, hyperthermia and local chemotherapy, using a broadband light source. This was the first clinical study to demonstrate the efficacy of this three-pronged anticancer strategy. The authors propose that this light-based approach should be considered as an adjuvant therapy (following surgery) for treating animals with soft-tissue sarcomas in veterinary medicine, as reported in the March 2014 Journal of Veterinary Science.
READ MORE to learn about other successful applications of PDT in veterinary medicine.
Support us by buying our book, The Medicine of Light, and ebooks from our Photoimmune Discoveries eBook Series.
Sources
Zhang X, Liu T, Li Z, Zhang X. Progress of photodynamic therapy applications in the treatment of musculoskeletal sarcoma (Review). Oncol Lett. 2014 Oct;8(4):1403-1408
Perentes JY, Wang Y, Wang X, Abdelnour E, Gonzalez M, Decosterd L, Wagnieres G, van den Bergh H, Peters S, Ris HB, Krueger T. Low-Dose Vascular Photodynamic Therapy Decreases Tumor Interstitial Fluid Pressure, which Promotes Liposomal Doxorubicin Distribution in a Murine Sarcoma Metastasis Model. Transl Oncol. 2014 May 13. [Epub ahead of print]
Onoyama M, Tsuka T, Imagawa T, Osaki T, Minami S, Azuma K, Kawashima K, Ishi H, Takayama T, Ogawa N, Okamoto Y. Photodynamic hyperthermal chemotherapy with indocyanine green: a novel cancer therapy for 16 cases of malignant soft tissue sarcoma. J Vet Sci. 2014;15(1):117-23.
Kaplan MA, Ol’shevskaya VA, Osipchuk YS, Nikitina RG, Kalinin VN. Photodynamic therapy of experimental sarcoma M-1 with boronated chlorine as a photosensitizer. Bull Exp Biol Med. 2014 May;157(1):74-6.
© Copyright 2014, Photoimmune Discoveries, BV




 English
English Français
Français Deutsch
Deutsch Nederlands
Nederlands