Pancreatic Cancer: Lighting Up Lymph Node Metastases
The pancreas is a long and fairly flat organ located deep in the belly. Part of the organ lies between the stomach and the spine, while another part is nestled in the curve of the upper small intestine. Because we can’t see or feel the pancreas in our daily lives, it’s easy to totally miss the growth of a tumor in the organ. We can’t know that cancer exists in the pancreas simply by pressing on the belly. Only when the tumor becomes large enough to interfere with the function of nearby structures, such as the liver or stomach, do we pay a visit to the doctor and eventually get handed a diagnosis of pancreatic cancer.
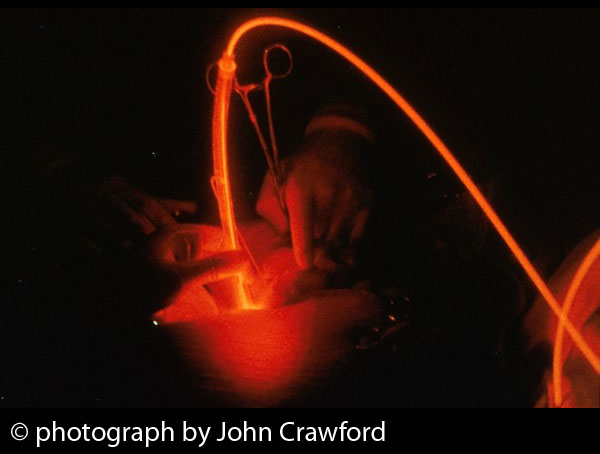
Pancreatic cancer is an aggressive disease that often spreads to the bile duct and duodenum, as well as to lymph nodes in the belly area. These metastases are found in the vast majority of pancreatic cancer cases, and they contribute a great deal to the lethal reputation of this disease. As we mentioned in Part 1, surgery is often very difficult and can be enhanced by the addition of photodynamic therapy, or PDT. PDT can also help overcome the resistance to conventional chemotherapy and radiotherapy.
What we didn’t mention is that the difficult surgery and resistance to conventional treatments also contribute to the high frequency of lymphatic metastases seen in pancreatic cancer. This means that the cancer spreads to the lymphatic system, the system that filters or helps clean the blood stream.
One way to detect these lymphatic metastases is by using tracer agents. These are agents that reveal the presence of cancer upon exposure to some source of energy, such as light or x-ray radiation. This detection, in turn, can facilitate the development of treatment options for the given diagnosis. At the present time, however, there is no ideal imaging method for the accurate detection of lymphatic metastases.
It turns out that the very same photosensitizers that may be used in the light-based treatment of pancreatic cancer also can serve as tracer agents to detect the lymphatic metastases. Scientists at Fudan University in Shanghai (China) recently conducted an animal study using the novel photosensitizer called deuteporfin as a tracer agent to detect lymphatic metastases in pancreatic cancer. They observed that the agent showed a much higher concentration in cancerous compared to normal tissues in the pancreas, as reported in the September 2015 issue of Oncology Letters.
What the Study Found
In this study, intravenous administration of the agent was found to be more practical—being easier to administer and also metabolized more rapidly—than the local lymphatic route. After being administered intravenously, deuteporfin levels rose rapidly in the pancreas and nearby lymph nodes. Impressively, the agent appeared to be “selectively enriched” in the cancerous pancreatic lymph nodes.
“These results indicated that deuteporfin may be developed as a novel photosensitizer tracer agent for the detection of lymphatic metastases in pancreatic cancer,” the Shanghai authors wrote. “The advantages of deuteporfin are that it has a selective tumor-targeting effect due to high tissue uptake, and that it may be administered intravenously and is therefore suitable for surgery.”
This appears to be the first published study of a photosensitizer being used as a tracing agent for the detection of lymphatic metastases of pancreatic cancer. Whether deuteporfin is truly useful as a tracer agent for detecting these metastases now needs to be evaluated in clinical studies of patients with pancreatic cancer.
It’s worth noting that the development of lymph node-specific PDT could eventually offer an alternative to the surgical removal of lymph nodes, a common practice in cancer treatment today. This is because studies have shown that such “anti-lymph node PDT” can help the lymph nodes undergo regeneration following treatment. Such regeneration of the lymph nodes would be enabled by altering the light fluence (intensity) and photosensitizer dose, as reported in the April 2014 issue of Angiogenesis.
Despite modern oncology’s best efforts, pancreatic cancer continues to be an extremely lethal disease, with the number of newly diagnosed patients nearly matching that of deceased patients. Fewer than 5% of all pancreatic cancer cases can be successfully treated with surgery, and approximately that same dismal percentage of patients will be alive five years later. Clearly the need for innovative approaches such as EUS-guided PDT and photodynamic diagnosis has never been greater.
Sources
Zhang D, Liu H, Wei Q, Zhou Q. Structure-activity relationship study of anticancer thymidine-quinoxaline conjugates under the low radiance of long wavelength ultraviolet light for photodynamic therapy. Eur J Med Chem. 2016 Jan 1;107:180-91.
Related Posts
-
 Boosting Anti-Cancer Immunity with Light
No Comments | Jan 21, 2016
Boosting Anti-Cancer Immunity with Light
No Comments | Jan 21, 2016 -
 Photoimmune Ways to Kill Cancer
No Comments | Jan 23, 2016
Photoimmune Ways to Kill Cancer
No Comments | Jan 23, 2016 -
 Using PDT to Cut Costs and Prevent Skin Cancer
No Comments | Feb 28, 2014
Using PDT to Cut Costs and Prevent Skin Cancer
No Comments | Feb 28, 2014 -
 Light-Based Conquest of Pancreatic Cancer
No Comments | Jan 26, 2016
Light-Based Conquest of Pancreatic Cancer
No Comments | Jan 26, 2016

 English
English Français
Français Deutsch
Deutsch Nederlands
Nederlands