Pancreatic Cancer: Clinical Research Provides New Hope
What does a cancer patient do when told that he or she has no other treatment options, and that the disease is too far advanced, perhaps even “terminal”? What if no standard treatment regimen exists for your particular cancer, or if the treatments recommended by your oncologist simply don’t seem to buy much survival time for you, the patient?
In most instances, the “terminal cancer” pronouncement is made when the oncologist perceives the disease to be overly aggressive and knows that there’s just not enough “gold standard” evidence to justify the choice of a particular treatment—even when that treatment has a wide margin of safety and has demonstrated considerable promise in some clinical studies.
The real challenge emerges when viewing cancers that are considered less common than, say, lung cancer or breast cancer. One of the classic examples here is pancreatic cancer, which in most cases refers to adenocarcinoma of the pancreas. This is a major cause of cancer-related death in Europe and North America. Even after surgery, the median survival is only about 15 months. Fewer than one in three patients will survive five years on average.
The majority of these cases involve cancer that has spread beyond the pancreas. It is generally believed that chemotherapy is the only treatment option for patients with these invasive cancers. Combining gemcitabine (brand name, Gemzar®) with other chemotherapy drugs is the current standard of care, though overall survival rates are still dismal.
Against this backdrop, it’s quite understandable that so many cancer patients would be clamoring to learn about nontoxic, minimally invasive treatment options that are capable of destroying the tumor. Such treatments could prove especially useful in situations in which surgery or other conventional strategies are likely to fall short.
Photodynamic Advantages: What Lab Research Is Finding
Photodynamic therapy (PDT) is a light-based method for destroying the tumor. The method entails the administration of a photosensitizing (light-sensitizing) agent that causes the tumor’s breakdown with the help of highly reactive molecules of oxygen known as singlet oxygen. This so-called photochemical reaction results in very little damage to the normal tissues and moreover helps activate the anti-cancer immune defenses.
In recent years, an impressive body of laboratory research has documented the potential benefits of PDT for pancreatic cancer. Some studies involved different pancreatic cell lines and showed that PDT killed those cells quite effectively. Other investigations showed that PDT was able to produce substantial shrinkage or destruction of tumors in animal models for pancreatic cancer.
Sodium alginate is a substance isolated from brown seaweeds. Recently, the field of nanotechnology has developed a “photosensitizer-encapsulated sodium alginate derivative” called Photosan-CSAD. This agent enters cancer cells very easily and has been shown to produce a very high fluorescence (glow) in pancreatic cancer cells. Researchers from Sun Yat-Sen University in Guangzhou, China, concluded that Photosan-CSAD is a candidate for the PDT of pancreatic cancer, as reported in the October 2014 International Journal of Pharmaceutics.
The possibility that PDT could knock out microscopic clusters of cells (micrometastases) via an effect on the anti-cancer immune mechanisms is another angle in need of further study. Recall that metastases are the primary basis for pancreatic cancer’s aggressive behavior. What’s needed here is a PDT strategy that can exploit these mechanisms while also targeting the tumor more directly.
The photosensitizer called Bremachlorin® could fill the bill in this regard. Bremachlorin-PDT can activate the anti-cancer immune mechanisms while also directly targeting the tumor and even cutting off the blood supply to the tumor. This is agent accumulates very strongly in tumors and is virtually free of side effects.
There is an urgent need to set up clinical trials to assess the therapeutic potential of such versatile, photoactive agents for the treatment for pancreatic cancer. The Natural Health Foundation has been striving to bring Bremachlorin-PDT to the European marketplace, and the initial findings have been very promising. It is hoped that such medicines will become more widely available in the near future.
Testing Different Photosensitizers in the Clinic
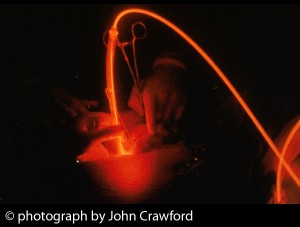
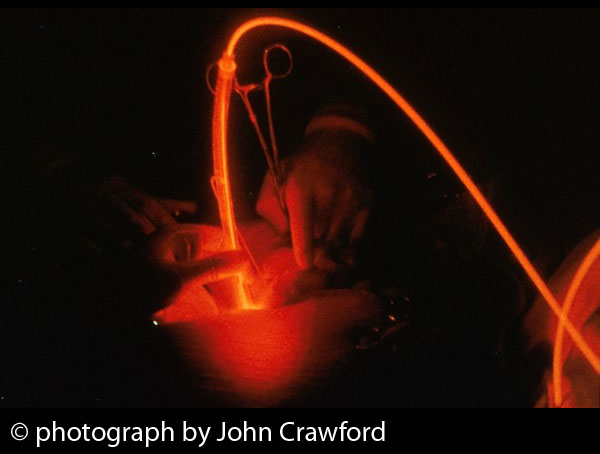
In a previous Discoveries article, we reported on the first-ever clinical trial of PDT for pancreatic cancer. Conducted at the National Medical Laser Centre in London, the study used a photosensitizer called meso-tetrahydroxyphenylchlorin, or mTHPC (marketed under the name, Foscan®). The study enrolled 16 patients with locally advanced pancreatic cancer, all of whom were treated with PDT. Light was delivered directly into the tumors via laser fibers that were passed through needles inserted in the skin.
Using computed tomography, all patients were found to have areas of tumor breakdown within a few days of receiving Foscan-PDT. All but two patients were discharged from the hospital within ten days.
The scientists concluded that PDT could produce the breakdown of pancreatic tumors, although special care was required for tumors invading nearby tissues. They also concluded that the median survival for these patients (9.5 months) was quite favorable. One patient was still alive after 31 months.
Verteporfin (trade name, Visudyne®) is a second-generation photosensitizer that has been licensed for the treatment of age-related macular degeneration, the primary cause of blindness in many countries. This agent is cleared from the body more rapidly than Foscan, and thus it does not result in the same level of skin sensitivity to light. (Note: Foscan’s main disadvantage is that patients must wait up to four days after receiving the drug before undergoing light treatment. Foscan-PDT also results in prolonged sensitivity of skin and eyes to light, and most patients need to stay out of bright sunlight for up to a month.)
In addition to its impressive safety, verteporfin displays an excellent capacity for absorbing and transmitting light energy, and this results in excellent tissue penetration. This means that verteporfin-PDT is appropriate for treating the deeper tumors found in solid organs like the pancreas. Lab studies have confirmed these effects on pancreatic tumors.
Dr. Bown’s first clinical research findings with verteporfin-PDT were impressive enough to garner approval for the conduct of additional clinical trials. Bown research team had also observed that even when PDT damages normal tissue, the treated areas can heal safely and without a significant loss of structure or function. These efforts have led to a more careful clinical assessment of PDT’s potential for treating pancreatic cancer.
The Second Clinical Trial: Putting Verteporfin to the Test
This year, Dr. Stephen Bown and colleagues at the National Medical Laser Centre in London (UK) collaborated with an international team of scientists on a clinical study of pancreatic cancer. They reported on a clinical trial of 15 patients with locally advanced pancreatic cancer. The investigators were from University College London (UK), Dartmouth College (USA), and Harvard Medical School’s Wellman Center for Photomedicine (USA). This trial used verteporfin (trade name Visudyne) as the photosensitizer for PDT of pancreatic cancer that could not be removed by surgery.
Again, the researchers chose verteporfin-PDT because it appears to have fewer side effects compared to the Foscan-PDT they had studied previously. The primary objective was to determine whether verteporfin-PDT is a safe treatment for patients with locally advanced, inoperable pancreatic cancer.
One hour after the verteporfin injection, the doctor aimed a low-power, red laser light at the pancreatic tumor. This was accomplished by passing fiberoptics (light fibers) through the skin and into the pancreatic tumor with the help of ultrasound or a CT scan to guide the placement of the fibers. In principle, the laser light activates the drug, which subsequently destroys the tumor cells.
This study had an exploratory aspect to it in that different amounts of light were tried. Of the 15 people in the trial, 13 had one fiber inserted; the first few received a small dose of laser light, the next few received more laser light, and so on until the right “light dose” was established. Of the two remaining people, one received two light fibers while the last person had three light fibers inserted.
In this clinical study, very few side effects were reported for the verteporfin-PDT. Only three people in the study reported mild to moderate belly aches after treatment, and the discomfort was easily cleared by taking painkillers. The average length of survival time was 15.5 months, as reported in the 2 April 2014 British Journal of Cancer.
The new findings suggest that verteporfin-PDT can be safely administered to people with pancreatic cancer that had spread to the surrounding body tissues. Subsequently, the same research team also showed that the verteporfin-PDT can be delivered with a much shorter drug-light interval and with less photosensitivity than with PDT protocols that used the older photosensitizers.
A shorter drug-light interval means that less times is needed for the photosensitizing agent to accumulate in the tumor. This advantage could make verteporfin-PDT a more practical and desirable approach for physicians who do not want to wait for several hours for the agent to perform its photodynamic duty, as reported by Dutch researchers recently reported in the February 2015 British Journal of Surgery.
Support us by buying our book, The Medicine of Light, and ebooks from our Photoimmune Discoveries eBook Series.
Sources
Yu Z, Li H, Zhang LM, Zhu Z, Yang L. Enhancement of phototoxicity against human pancreatic cancer cells with photosensitizer-encapsulated amphiphilic sodium alginate derivative nanoparticles. Int J Pharm. 2014 Oct 1;473(1-2):501-9.
Rombouts SJ, Vogel JA, van Santvoort HC, van Lienden KP, van Hillegersberg R, Busch OR, Besselink MG, Molenaar IQ. Systematic review of innovative ablative therapies for the treatment of locally advanced pancreatic cancer. Br J Surg. 2015 Feb;102(3):182-93.
© Copyright 2015, Photoimmune Discoveries, BV




 English
English Français
Français Deutsch
Deutsch Nederlands
Nederlands