Lighting Up Aggressive Brain Cancer, Part 1
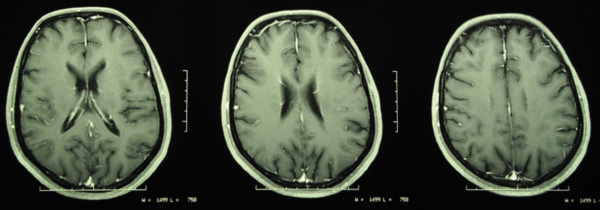 Brain cancer is often a deadly diagnosis. In 2008, approximately 238,000 new cases of brain tumors were diagnosed worldwide, with an estimated 175,000 deaths. Glioblastoma is the most common primary brain tumor, as well as the deadliest. In particular, glioblastoma multiforme (GBM) presents a grave challenge in the treatment and management of cancer patients worldwide.
Brain cancer is often a deadly diagnosis. In 2008, approximately 238,000 new cases of brain tumors were diagnosed worldwide, with an estimated 175,000 deaths. Glioblastoma is the most common primary brain tumor, as well as the deadliest. In particular, glioblastoma multiforme (GBM) presents a grave challenge in the treatment and management of cancer patients worldwide.
Even with aggressive surgery—taking advantage of state-of-the-art preoperative and intraoperative neuroimaging, along with recent advances in radiotherapy and chemotherapy—the outlook for GBM patients remains dismal, with average survival being only a year from the time of diagnosis and most patients dying within two years. Much remains unknown as to why some patients survive longer with GBM.
A key aspect of brain tumor biology that continues to stymie therapeutic progress is the spreading of the brain tumor into surrounding normal brain tissues—that is, into areas well away from the main tumor mass. Photosensitizers can localize in other areas as well as the main tumor mass. This allows the cancer surgeon to see areas that can treated surgically or that could be exposed to light during photodynamic therapy (PDT).
The ideal photosensitizers in this situation would be actively taken up by tumor cells, but activated by light of a longer wavelength, result in greater tissue penetration and consequently more complete eradication of tumor cells that have migrated into surrounding normal brain (away from the main tumor mass). The NHF has been actively involved in supporting the development of photosensitizers for this purpose.
In a recent clinical study of GBM patients treated with PDT, the 12-month overall survival and six-month progression-free survival were both 100%. The purpose of this study was simply to assess the potential efficacy and safety of intraoperative PDT using talaporfin sodium (the photosensitizer) and a 664-nm semiconductor laser in patients with primary malignant parenchymal brain tumors, including GBM. (The Natural Health Foundation has supported studies of various photosensitizers to help establish optimal treatment protocols.)
The researchers concluded that the use of intraoperative PDT in a combined treatment strategy may have a positive impact on overall survival and local tumor control for patients with newly diagnosed GBMs. This study was conducted at the Tokyo Women’s Medical University in Japan and reported in the 16 August 2013 Journal of Neurosurgery. Of course, the real question is what happens to these patients over the long term, and follow-up reports on this group of patients will be eagerly awaited.
One of the most aggressive forms of brain cancer is recurrent or high-grade GBM (WHO grade IV). For this form of GBM, the median survival is only three months with standard therapy. According to a 2005 study reported in the Journal of Clinical Neuroscience, however, the median survival for recurrent GBM patients treated with PDT may be closer to 15 months. If future studies confirm this result, this indicates that PDT may be five times more effective than the current standard therapy.
In Part 2, we report on the most recent analysis of all the survival data to date, and explain how future research can better illuminate the role of fluorescence-guided surgery and PDT in the treatment of malignant brain tumors.
Support us by buying our book, The Medicine of Light, and ebooks from our Photoimmune Discoveries eBook Series.
Sources
Muragaki Y, Akimoto J, Maruyama T, Iseki H, et al. Phase II clinical study on intraoperative photodynamic therapy with talaporfin sodium and semiconductor laser in patients with malignant brain tumors. J Neurosurg. 2013 Aug 16. [Epub ahead of print]
Kanu OO, Mehta A, Di C, Lin N, Bortoff K, Bigner DD, Yan H, Adamson DC. Glioblastoma multiforme: a review of therapeutic targets. Expert Opin Ther Targets. 2009;13(6):701-18.
Stylli SS, Kaye AH, MacGregor L, Howes M, Rajendra P. Photodynamic therapy of high grade glioma – long term survival. J Clin Neurosci. 2005;12(4):389-98.
© Copyright 2013, Photoimmune Discoveries, BV


 English
English Français
Français Deutsch
Deutsch Nederlands
Nederlands