PDT: A More Focused Approach to Prostate Cancer
Around the world, prostate cancer has now overtaken lung and colon cancers as the most common type of cancer found in men. It is by far the most common cancer among men in Europe, North America, and many industrialized nations. This year, an estimated one million new cases will be diagnosed worldwide.
Though many cases of prostate cancer can be treated early and are thus highly curable, a large number of cases are fatal. Also, the usual treatments for early-stage prostate cancer result in either total loss of the prostate or damage to normal, healthy tissue. Either way, the treatments can have negative consequences for a man’s quality of life.

At the present time, for example, many men who undergo either radical prostatectomy or radiotherapy can expect to experience problems such as erectile dysfunction and an inability to have sexual intercourse. Others will experience an increase in urinary incontinence and in some cases problems with bowel function as well.
Any approach that minimizes such side effects is worth exploring. This is why increasing interest has come to bear on using various kinds of focal therapy for prostate cancer—therapies that are more focused on the cancer itself, and less likely to cause damage to the normal prostate tissue or to other surrounding tissues such as the sphincter and neurovascular bundles.
PDT as an Emerging Focal Therapy for Prostate Cancer
Focal therapy is a tissue- and organ-preserving approach that offers men the potential for treating their localized prostate cancer without the side effects associated with radical surgery or radiation treatments. Technically, focal therapy therapies is most effective in treating patients who have unifocal and low-volume prostate cancer.
Three examples of focal therapy are as follows: (1) Photodynamic Therapy (PDT), the use of a light-sensitizing agent that absorbs and transmits light’s energy in order to destroy malignant cells; (2) Cryosurgery, the freezing of the prostate tissue in order to kill the cancer; and (3) High-Frequency Focused Ultrasound (HIFU), the use of high-energy sound waves then heat and destroy cancer cells in that area.
Like HIFU, PDT can be used to target the cancer very specifically while largely sparing normal, healthy tissues. This leads to excellent outcomes in terms of overall functioning and quality of life, especially when compared to conventional surgery and radiotherapy. Unlike HIFU and cryotherapy, PDT does not require the use of expensive machines. As a non-invasive form of focal therapy, PDT can efficiently eliminate the disease while minimizing the treatment burden posed by more invasive methods, as reported in the August 2014 issue of Urologic Oncology.
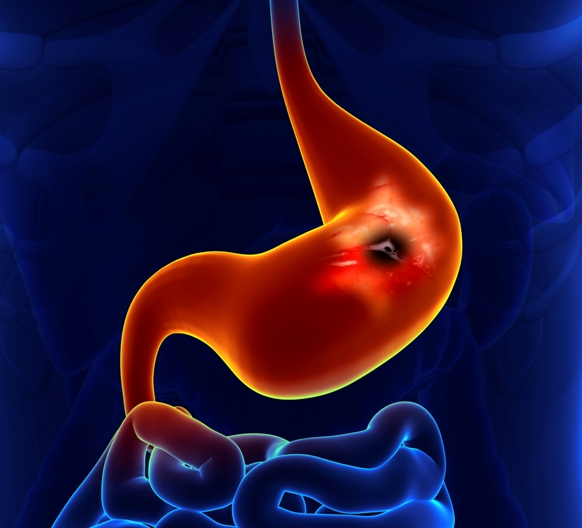
The Basics of PDT for Prostate Cancer
In the PDT approach, light can be used to treat either the entire gland or small tumors within the gland. With the whole gland approach, light can be effectively delivered under ultrasound guidance to the entire prostate gland using special optical fibers. The fibers are inserted into the prostate using a standard brachytherapy grid. Alternatively, using modern imaging technology, these small light-delivering probes can be positioned in the prostate to deliver PDT to specific portions of the gland.
In addition, the use of near-infrared light triggered PDT may lead to a synergy of both photothermal and photodynamic treatment effects. This combination therapy may represent a highly effective treatment for prostate cancer, as reported in the 7 April 2014 issue of Molecular Pharmacology.
The therapeutic target can also include the vascular bed that directly supports the prostate. A photosensitizing agent is injected intravenously and is distributed throughout the body. The PDT’s light reaction selectively destroys the vascular supply to prostate tumors, causing them to shrink and die. This latter approach is referred to as vascular-targeted PDT. Recent clinical studies have reported that at least 83% of biopsies are negative six months after this treatment, and the treatment is well tolerated, as reported in the 3 September 2014 issue of Progrès en Urologie, a French medical journal.
Toward More Effective Focal Therapy
At this time, only about 10% of men diagnosed with low-risk, localized prostate cancer choose watchful waiting as their initial treatment; the rest choose treatment. Nonetheless, as the incidence of localized prostate cancer continues to rise on a global scale, the standard radical treatments for localized prostate cancer have been questioned due to their associated complications, side effects, costs, and limited ability to guarantee remissions over the long term. PDT focal therapy may prove to be an effective alternative strategy, as men with low-risk tumors (low-grade, non-aggressive) are likely to benefit the most from this approach
PDT stands in sharp contrast with surgery in that it tends to have the opposite impact on metastasis. This is because PDT produces an acute inflammatory effect that, in turn, helps bring about a strong anti-cancer immune response, one that actually works against the growth of metastases. These immune effects have been extensively studied and are carefully explained in our book, The Medicine of Light. Though these effects are still being mapped out with respect to prostate cancer, it stands to reason that PDT could offer a strong alternative to surgery in certain situations as determined by your medical team.
PDT for prostate cancer is now considered in the same group of focal therapy options as cryotherapy, high-intensity focused ultrasound, and photothermal therapy. All of these modalities can precisely treat prostate tumors to within a few millimeters, thus minimizing damage to the surrounding tissues. Aside from the lack of side effects (at least compared to surgery and radiation), PDT may result in better long-term control of the disease because of its favorable effects on anti-cancer immunity. Clinical trials are needed to test this assertion.
Support us by buying our book, The Medicine of Light, and ebooks from our Photoimmune Discoveries eBook Series.
Sources
Marien A, Gill I, Ukimura O, Nacim B, Villers A. Target ablation-Image-guided therapy in prostate cancer. Urol Oncol. 2014 Aug;32(6):912-923.
Lebdai S, Martin F, Bigot P, Azzouzi AR. Treatment of localized prostate cancer by vascular-targeted photodynamic therapy with WST11. [Article in French] Prog Urol. 2014 Sep 3. [Epub ahead of print]
Fan Z, Dai X, Lu Y, Yu E, Brahmbatt N, Carter N, Tchouwou C, Singh AK, Jones Y, Yu H, Ray PC. Enhancing targeted tumor treatment by near IR light-activatable photodynamic-photothermal synergistic therapy. Mol Pharm. 2014 Apr 7;11(4):1109-16.
Ahmed HU, Berge V, Bottomley D, Cross W, Heer R, Kaplan R, et al. Prostate Cancer RCT Consensus Group. Can we deliver randomized trials of focal therapy in prostate cancer? Nat Rev Clin Oncol. 2014 Aug;11(8):482-91.
© Copyright 2014, Photoimmune Discoveries, BV



 English
English Français
Français Deutsch
Deutsch Nederlands
Nederlands