Overcoming Colorectal Cancer with PDT: New Insights
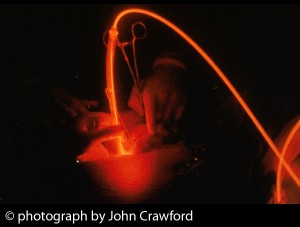
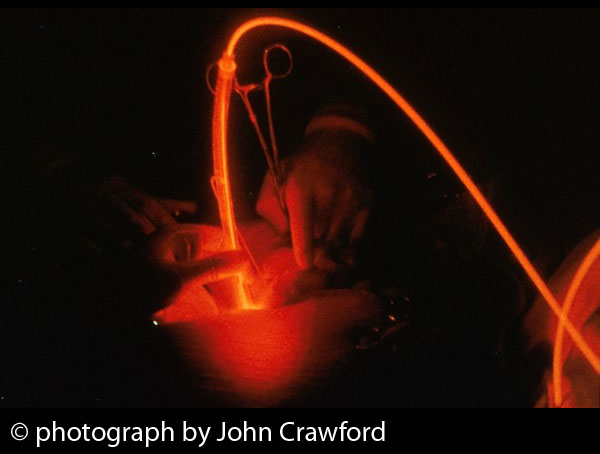
Colorectal cancer, a malignant disease of the colon and rectum, gradually develops over the course of several decades and is a leading cause of cancer-related death in most Western countries. Given the hollow structure of the colon, and the easy access to the anus and rectum, it would seem logical to assume that photodynamic therapy, or PDT, could be a useful treatment for colorectal cancer. PDT entails the use of a light-sensitizing agent, or photosensitizer, followed by illumination of the tumor with visible light; this leads to the production of reactive oxygen species (chemically reactive molecules containing oxygen) that cause direct damage to the tumor as well as the blood vessels supporting the tumor.
But while numerous studies have explored the use of PDT as a way to remove colon polyps (which may increase the risk of colorectal cancer), relatively few studies have assessed the effects of PDT for colorectal tumors. This may be due to the assumption that surgery will produce good outcomes with early-stage colorectal cancer (and of course polyps), and that laser therapy and stents alone can be effective. Laser therapy, using a laser to kill cancer cells, is regarded as a specialized surgical treatment that may be able to destroy bowel cancer that has spread to the liver.
Nevertheless, PDT may offer some distinct advantages over both surgery and conventional laser therapy. Unlike laser treatment, healing from PDT occurs with less scarring, and because collagen is preserved during PDT, there is no reduction in the mechanical strength of the colon. According to early studies done in the 1980s and 1990s, PDT produced favorable response rates and good symptomatic relief and recovery in colorectal cancer patients.
Most of the reports on PDT and photoimmunotherapy (PIT) to date have come from experimental studies taking place in laboratory experiments in which the photodynamic methods either killed colon cancer cells in the test tube or blocked the growth of colon tumors in animals. And even relatively inexpensive light sources such as light-emitting diodes (LEDs) have been shown to be effective in these experimental situations.
The most recent experiments, conducted at Tottori University in Tottori, Japan, focused on the possibilities of combining PDT with hyperthermia, an approach they refer to as photodynamic hyperthermal therapy (PHT). Hyperthermia involves heating up the tumor (or whole body, in some cases), and it has become a major treatment strategy for colorectal cancer.
The Japanese study used a light-sensitizing agent called indocyanine green (ICG) and a broadband light source in order to treat mice with colon tumors. The other groups were administered either ICG alone (ICG group), light alone (light group) or no treatment (control group). Following the treatment, tumor growth was measured. In the PHT group, the tumor growth rates were significantly lower compared with those observed in the other groups. Markers of tumor cell proliferation were also markedly lower in the PHT group compared to the control and ICG groups. These data indicate that PHT may offer an effective option for treating colorectal tumors, as reported in the April 2014 issue of Oncology Letters.
A second set of experiments was conducted by an international team of scientists from the United States, Poland and the Netherlands. This study focused on the effects of PDT on the immune system. It is known that, in addition to its direct tumor-killing effects, PDT bolsters the body’s anti-cancer immunity by improving the immune system’s ability to recognize the tumor. The researchers showed that the anti-tumor immune response is further improved when PDT is combined with a clinically approved drug called decitabine (5-aza-2′-deoxycytidine). This drug results in further modification of tumor antigens, proteins that are picked up and (ideally) recognized as a threat by the immune system.
In animal studies of both colon cancer and breast cancer, this combination therapy resulted in complete responses and long-term survival. Moreover, all long-term surviving mice were able to resist re-inoculation with the same tumor cells, suggesting protection against relapses. The international team concluded that PDT leads to strong specific antitumor immune responses, and that this combined strategy may be a novel approach to further enhance the effectiveness of PDT, as reported in the May 2014 European Journal of Cancer.
Researchers from the University of Oslo (Norway) are using nanotechnology (nanovehicles of Pluronics) in an attempt to improve the delivery of various photosensitizers to the tumors. Their research suggests that this technology may improve the efficacy of porphyrin-based photosensitizers, as reported in the January 2014 issue of Photochemical & Photobiological Sciences.
Though PDT may prove to be a highly effective approach to cancer therapy, it does have its limitations, too. There are multiple mechanisms involved in the regulation of cancer cell death that can be successfully targeted for further improvement of PDT, at least in individual cases. Along these lines, Researchers from the Institute of Biology and Ecology, in Košice, Slovak Republic, showed last year that control of the redox state of the cancer cell—that is, the dynamic balance of antioxidants and free radicals within the cell—could help determine the success of PDT against cancer, as reported in the December 2013 issue of Photodiagnosis and Photodynamic Therapy. Many studies are currently under way to help scientists understand why some patients may respond better than others to this light-based therapy.
Support us by buying our book, The Medicine of Light, and ebooks from our Photoimmune Discoveries eBook Series.
Sources
Onoyama M1, Azuma K2, Tsuka T3, Imagawa T3, Osaki T2, Minami S2, Ogawa N4, Okamoto Y5. Effects of photodynamic hyperthermal therapy with indocyanine green on tumor growth in a colon 26 tumor-bearing mouse model. Oncol Lett. 2014 Apr;7(4):1147-1150.
Sobczyński J1, Kristensen S, Berg K. The influence of Pluronics nanovehicles on dark cytotoxicity, photocytotoxicity and localization of four model photosensitizers in cancer cells. Photochem Photobiol Sci. 2014 Jan;13(1):8-22.
Saavedra R, Rocha LB, Dąbrowski JM, Arnaut LG. Modulation of biodistribution, pharmacokinetics, and photosensitivity with the delivery vehicle of a bacteriochlorin photosensitizer for photodynamic therapy. ChemMedChem. 2014 Feb;9(2):390-8.
Mikešová L1, Mikeš J, Kovaľ J, Gyurászová K, Culka L, Vargová J, Valeková B, Fedoročko P. Conjunction of glutathione level, NAD(P)H/FAD redox status and hypericin content as a potential factor affecting colon cancer cell resistance to photodynamic therapy with hypericin. Photodiagnosis Photodyn Ther. 2013 Dec;10(4):470-83.
© Copyright 2014, Photoimmune Discoveries, BV



 English
English Français
Français Deutsch
Deutsch Nederlands
Nederlands