Prostate Cancer: A Saner, More Conservative Approach
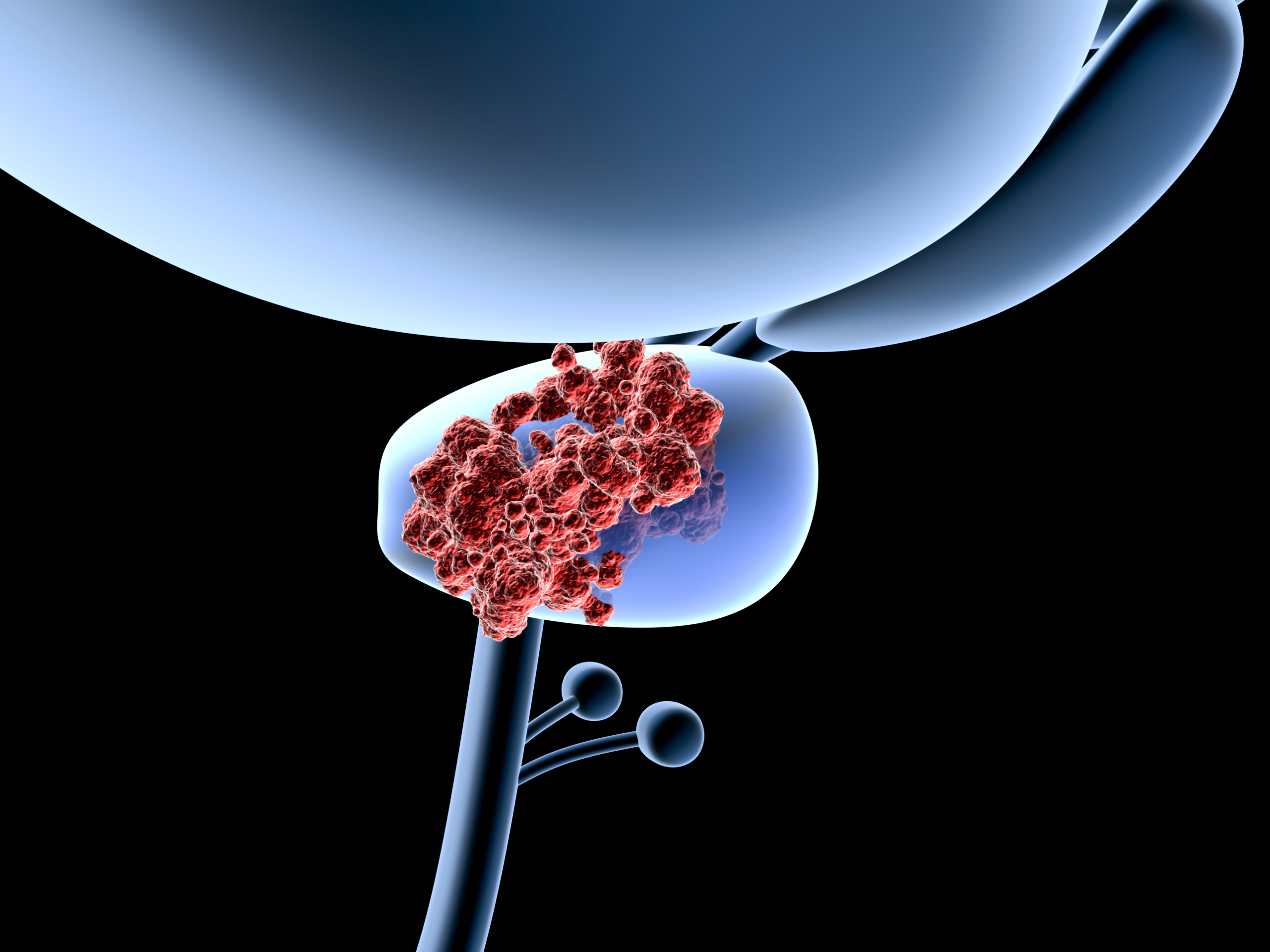
Prostate cancer is the most prevalent form of cancer among men in Europe, with an incidence that has increased rapidly over the past two decades. These tumors develop slowly over the course of a man’s lifetime, and millions of men grow old without knowing that they’ve been harboring such growths. Indeed, autopsy studies have shown that most elderly men die from other causes, totally unaware that they ever had prostate cancer.
Since the introduction of PSA screening in the 1980s, millions of early-stage prostate tumors have been detected that would never have caused symptoms. These tumors are usually treated with either surgery or radiotherapy, treatments that result in the loss of the prostate gland or at least major damage to prostate tissues.
Even though most of these tumors would never progress to become a lethal disease, the majority of men will opt for treatments that often lead to erectile dysfunction (impotence) and loss of bladder control.. This decision usually arises from fear that the disease could become life-threatening.
For men with a local recurrence of prostate cancer, surgery is often considered the best first option. But while removal of the prostate can lead to long-term cancer control, the operation is often technically challenging and linked with significant complications. Hormonal therapy and brachytherapy (a type of radiation treatment) are also used in such situations, but these treatments are not curative.
More recently, oncologists have begun considering less invasive approaches, such as photodynamic therapy (PDT), cryotherapy and high-intensity focused ultrasound (HIFU). These treatments can destroy the cancer with minimal damage to the surrounding normal tissues. PDT may have some unique advantages because of its ability to also activate the immune system against metastases or disease that extends beyond the primary tumor.
Targeting the Tumor’s Blood Supply
As a minimally invasive technique, PDT combines an injection of a photosensitizing agent with exposure of the target tissue to light. This results in the generation of reactive oxygen molecules that, in turn, trigger the death of cancer cells. Various photosensitizing agents have demonstrated promising results in clinical trials for prostate cancer.
Some of these agents enable the PDT to damage the blood vessel supply to the tumor, an approach known as vascular-targeted photodynamic therapy. One such agent is WST11 (TOOKAD® Soluble), which is injected intravenously prior to light treatment. With the patient under general anesthesia, light fibers are introduced through the abdomen (perineum) into the prostate, with the procedure usually guided by ultrasound. This is followed by focusing laser light on the target area.
Recent studies suggest that vascular-targeted PDT may offer a successful treatment strategy for prostate cancer. A clinical trial of 40 men showed that vascular-targeted PDT with WST11 resulted in a negative biopsy rate of 83% after six months. This favorable outcome was nearly twice the negative biopsy rate of the control groups, as reported online ahead-of-print in the 19 May 2014 issue of BJU International. In addition, the treatment was well tolerated.
The ideal photosensitizing agent would not only target the tumor’s blood supply but also offer other lines of attack. One promising agent in this regard is Bremachlorin®, which is now undergoing scientific evaluation for eventual market authorization in Europe. This agent is unique in that it attacks the tumor directly, damages the tumor’s blood supply, and stimulates the anti-cancer immune defenses. Moreover, unlike many other photosensitizers, Bremachlorin-PDT is extremely well tolerated, with no need to avoid sunlight following the treatment.
Gauging the Success of Treatment
To determine whether the treatment is actually working, some researchers have proposed using magnetic resonance imaging (MRI). At this writing, several studies have shown that contrast-enhanced MRI can successfully demonstrate the breakdown of tumors following cryotherapy and HIFU, with an accuracy as high as 83%. For this reason, it was hoped that the same strategy could be used to monitor the response to PDT.
A recent study used an MRI to monitor the presence of disease following PDT in patients for whom radiotherapy had previously failed. This clinical trial used WST09 as the light-sensitizing agent for PDT. All of the patients had previously undergone the standard treatment known as external beam radiation therapy; however, their disease had continued to progress following radiotherapy.
Studies at the Central Hospital at the University of Angers (France) and at the Ontario Cancer Institute in Toronto, Ontario (Canada), demonstrated that MRI was able to successfully predict the early outcome of PDT in these patients. The sensitivity of the MRI for this purpose was 100%. The researchers also surmised that this method was much more reliable than using PSA to monitor the responses to PDT, as reported in the September-October 2014 Canadian Urological Association Journal.
Such information is important because it affects the physicians decision to retreat with PDT. If the MRI suggests that there is residual disease, then the photodynamic strategy could be repeated in order to stop the possible progression of the cancer.
PDT has certain advantages over surgery and other treatment strategies:
- It is less invasive than prostatectomy, and the treatment can usually be performed in an outpatient setting.
- Multiple treatment sessions can be performed without the dose limitations associated with radiotherapy.
- Following PDT, the tumor tissue can be readily identified by laboratory analysis of the tissue (histology), in contrast with the treatment effects of hormonal or radiation therapy, which can hamper such an analysis.
With the growing need for a more conservative approach to prostate cancer treatment, more and more men are interested in less invasive therapeutic strategies. PDT is certainly a viable option, one that should be considered alongside other so-called “focal therapies”, such as HIFU, cryotherapy, and interstitial laser thermotherapy, as reported in the August 2014 issue of Future Oncology. All of these therapies are now undergoing evaluation as ways to eliminate prostate cancer without compromising the man’s quality of life and peace of mind.
Sources
Kulik M, Nedelcu C, Martin F, Lebdai S, Rousselet MC, Azzouzi AR, Aubé C. Post-treatment MRI aspects of photodynamic therapy for prostate cancer. Insights Imaging. 2014 Oct 7. [Epub ahead of print]
Barrett T, Davidson SR, Wilson BC, Weersink RA, Trachtenberg J, Haider MA. Dynamic contrast enhanced MRI as a predictor of vascular-targeted photodynamic focal ablation therapy outcome in prostate cancer post-failed external beam radiation therapy. Can Urol Assoc J. 2014 Sep;8(9-10):E708-E714.
Lebdai S, Martin F, Bigot P, Azzouzi AR. Treatment of localized prostate cancer by vascular-targeted photodynamic therapy with WST11. [Article in French] Prog Urol. 2014 Sep 3. [Epub ahead of print]
Mazzucchelli R, Lopez-Beltran A, Galosi AB, Zizzi A, Scarpelli M, Bracarda S, Cheng L, Montironi R. Prostate changes related to therapy: with special reference to hormone therapy. Future Oncol. 2014 Aug;10(11):1873-86.
© Copyright 2014, Photoimmune Discoveries, BV




 English
English Français
Français Deutsch
Deutsch Nederlands
Nederlands