Breast Cancer: New Light on Chest Wall Recurrences
Breast cancer is the most common type of cancer in women worldwide, with nearly two million new cases diagnosed each year. The disease accounts for at least one in every 10 deaths from cancer in women. According to the World Health Organization, approximately 508,000 women died from breast cancer in 2011.
When breast cancer has not become invasive or has not spread elsewhere in the body, it can often be “cured” by surgery. On the other hand, breast cancer that has spread to the lymph nodes or other parts of the body is harder to treat, and advanced metastatic breast cancer (Stage IV) is considered to be an incurable or “terminal” disease in about 98% of all cases.
It has been estimated that up to 45% of all breast cancer surgeries may result in a recurrence, though the rate is considerably reduced for people who receive either radiation or chemotherapy or both. Most breast cancer recurrences take place within five years from the time of surgery. In general, these recurrences are more aggressive than the initial manifestation of the disease.
Many oncologists are interested in innovative strategies for overcoming these recurrences once they arise. Part of this interest may stem from the fact that more and more patients with recurrent breast cancer are asking for less toxic, more humane approaches. The light-based therapies discussed in the next section offer just such an option for these patients.
The Promise of Photodynamic Therapy
For thousands of years, light has been known to have profound therapeutic power. In the early 1900s, photodynamic therapy, or PDT, emerged as a way to harness light’s healing potential. The crux of the photodynamic approach is the use of a light-sensitizing agent, or photosensitizer, which reacts with light and oxygen. In a nutshell, the photosensitizing agent absorbs and transmits light’s energy in order to destroy abnormal cells, including cancer cells.
PDT is attractive as a breast cancer treatment for several reasons. First, it targets breast tumors while minimizing damage to normal tissues. Second, it can override the cancer cell’s resistance to chemotherapy and radiotherapy. Lastly, PDT can be combined with one or more of these treatments for a stronger tumor-killing effect—without the toxic side effects commonly associated with chemotherapy or radiotherapy.
PDT could also improve the treatment of breast cancer by compensating for some of the limitations of conventional surgery. In particular, as noted above, surgery’s frequent inability to eliminate all of the cancer cells in a particular area can lead to a recurrence or relapse later on. In some cases, these recurrences may respond more favorably to PDT than to standard treatments.
Light-Based Therapy for Chest Wall Recurrences
One type of breast cancer recurrence that can take place after the breast-removing surgery known as mastectomy is cancer in the chest wall. This phenomenon is fairly rare, occurring in only about 8% of all breast cancer cases. Nevertheless, it remains a very serious problem, and is much more common in poor or underserved populations, with an incidence as high as 60% in some breast cancer patient groups.
Patients with chest wall recurrences often face a very aggressive, metastatic disease situation that cannot be adequately controlled with conventional treatments. When methods such as surgery, radiotherapy, and chemo-hormonal therapy have fallen short, there are few established options available. This can lead to disabling feelings of hopelessness and despair for the patient.
Thankfully, PDT has emerged as a promising treatment option for chest wall recurrences. The basic approach uses a photosensitizer along with laser light to trigger the selective destruction of the metastases in the chest wall. The cancer breaks down mainly through the process of necrosis, which is also more favorable for triggering the anticancer immune defenses.
Favorable findings from a number of clinical studies attest to the claim that PDT can be an effective treatment for chest wall recurrences. The most recent example comes from a randomized clinical trial conducted at the National Clinical Research Center of Cancer in Tianjin, China. This trial enrolled 40 patients with recurrences to the chest wall in order to test the possibility that PDT could improve outcomes for these patients.
The 40 patients were divided into two groups. Group A received radiotherapy only, while group B received the combination of PDT and radiotherapy. The photosensitizer used in this study was 5-ALA, one of the older photosensitizer drugs. Forty-eight hours after administering the 5-ALA, red light was administered and then followed by radiotherapy one day later.
There was no statistically significant difference in the elimination of the chest wall recurrences between the two groups. The investigators speculated that this may have been due to the relatively small size of the study population, and that a larger clinical trial would be needed to adequately test PDT’s impact on chest wall recurrences.
On the other hand, more patients treated with the PDT-radiotherapy combination (group B) achieved a complete response within a shorter time period than those treated with radiotherapy alone (group A). The complete response rate was more than twice as high in group B as in group A (50% versus 20%, respectively), and this result was statistically significant. Also, whereas most patients in group B achieved a complete response in only 110 days, this same response took about 175 days for group A.
The Tianjin scientists point out that Group B’s shorter time to a complete response may translate into a better quality of life for PDT-treated patients. They further speculate that PDT may have interacted in a synergistic way with the radiotherapy. They note that the DNA or genetic material inside the cancer cell is the main target for ionizing radiation treatments, and PDT is known to cause several types of DNA damage by generating highly reactive oxygen molecules inside the cancer cell.
Finally, further analysis revealed that among patients who received PDT-radiotherapy, those without oozing scabs were more likely to respond to the therapy than those with oozing scabs. The authors suggest that the presence of oozing scabs could alter the treatment outcome because these scabs could influence the amount of light penetrating the skin to reach the cancer. Alternatively, the oozing scabs could indicate a low-oxygen condition that would also limit the effectiveness of PDT. Thus, removing the oozing scabs could potentially improve the therapeutic outcome of PDT.
In this study, the major side effect of PDT was skin sensitivity to light (also known as photosensitivity). This occurred in approximately one out of every five patients. The radiotherapy-related side effects included nausea, vomiting, skin redness (around the treatment site), itching and skin peeling. Nevertheless, the authors considered the combination treatment to be safe and urged further studies of the PDT-radiotherapy combination, as reported in the June 2014 Journal of Breast Cancer.
Evidence from a Pilot Study at Tufts University
Additional support for the use of PDT to treat chest wall recurrences comes from a study at Tufts University School of Medicine in Boston, Massachusetts (USA). Nine patients were diagnosed with clear evidence of chest wall progression of breast cancer following mastectomy. Previous treatment with surgery and radiotherapy had failed. In such cases, the use of subsequent radiotherapy is considered futile, hence the need for reasonable and responsible alternatives.
In this small pilot study, six of the nine patients (67%) showed either a complete or partial clinical response following PDT. Two of the patients showed a substantial tumor regression away from the field of treatment, possibly suggesting that PDT had activated the immune system against the cancer.
Of the eight patients for whom adequate test results were available, all eight (100%) demonstrated a clear response to treatment in terms of tumor shrinkage. At the same time, quality-of-life measures were improved following treatment, with less pain and bleeding from the tumor nodules.
These data indicate that PDT may be an effective, low-morbidity therapeutic option for the treatment of chest metastases of breast cancer following mastectomy. The authors propose that further evaluation in a larger group of patients would be warranted in order to better assess the treatment’s efficacy and to help further optimize the intervention, as reported in the December 2014 Journal of Surgical Research.
Support us by buying our book, The Medicine of Light, and ebooks from our Photoimmune Discoveries eBook Series.
Sources
Liu Y, Hou G, Zhang X, Liu JJ, Zhang S, Zhang J. A pilot randomized clinical study of the additive treatment effect of photodynamic therapy in breast cancer patients with chest wall recurrence. J Breast Cancer. 2014 Jun;17(2):161-6.
Feng X, Zhang Y, Wang P, Liu Q, Wang X. Energy metabolism targeted drugs synergize with photodynamic therapy to potentiate breast cancer cell death. Photochem Photobiol Sci. 2014 Dec 12;13(12):1793-803.
© Copyright 2014, Photoimmune Discoveries, BV
Related Posts
-
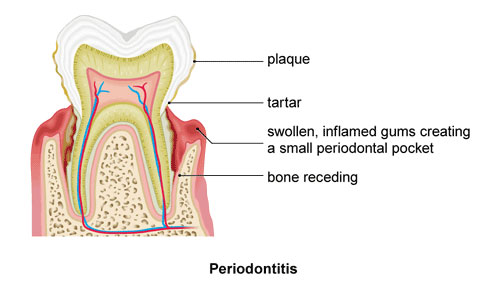 Overcoming Periodontal Disease with Light
No Comments | Oct 16, 2014
Overcoming Periodontal Disease with Light
No Comments | Oct 16, 2014 -
 Basal Cell Carcinoma: The Treatment Choice is Personal
No Comments | Jan 9, 2016
Basal Cell Carcinoma: The Treatment Choice is Personal
No Comments | Jan 9, 2016 -
 Hope for Herpes: The Power & Promise of PDT
No Comments | Jun 30, 2014
Hope for Herpes: The Power & Promise of PDT
No Comments | Jun 30, 2014 -
 Curing the Most Common Cancer: Basal Cell Carcinoma
No Comments | Oct 27, 2014
Curing the Most Common Cancer: Basal Cell Carcinoma
No Comments | Oct 27, 2014



 English
English Français
Français Deutsch
Deutsch Nederlands
Nederlands