Cervical Cancer Treatment: Can We Replace Surgery with Light?
When it comes to treating cancer, the first-line of attack from a conventional standpoint is to cut out the disease using surgery. One of the problems with surgery, however, is that it may damage the adjacent normal tissues and organ structures, potentially compromising a person’s functioning and overall quality of life For these and other reasons, there is increasing interest in exploring non-surgical treatment options.
A good example of the need for reasonable alternatives to surgical treatments involves cervical cancer, the second most common cancer among women worldwide. Though cancer of the cervix is most common in developing countries, incidence and mortality rates for a type of cervical cancer called cervical adenocarcinoma have been steadily rising in Europe and North America, especially among younger women. The largest increases in these rates have been seen in the United Kingdom, Iceland, Sweden, England, Spain, Finland, Slovakia, Slovenia, and the Netherlands.
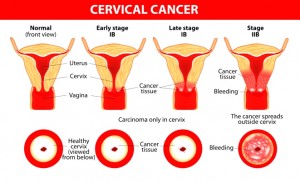
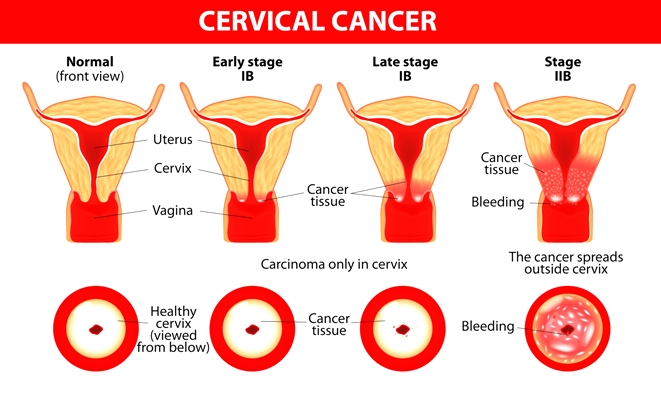
This particular cancer is thought to grow slowly in the interior lining of the cervix, usually developing over a period of years. The disease starts with precancerous changes in normal cells that can be relatively easy to detect. This cluster of abnormal cells is referred to as cervical intra-epithelial neoplasia or CIN. Though the condition itself is not cancerous, and many women with CIN do not develop cancer, the abnormal cells may lead to cancer.
Why Light-Based Alternatives Are Being Explored
The conventional approach is based on surgical excision, i.e., various ways of removing the diseased tissue. Common examples include loop electrosurgical procedure and the cold knife technique. Using these surgical methods, CIN is considered to be completely curable in most cases. The problem with these strategies is that they damage the cervix, which may in turn result in obstetrical problems in case a woman gets pregnant, notably an increased risk of morbidity and mortality for the newborn.
Photodynamic therapy, or PDT, offers a reasonable, minimally invasive alternative to surgery and is both safe and effective as a treatment for CIN. This innovative treatment involves administering a photosensitizing agent and then exposing the target tissue area to light of a specific wavelength. The resulting photochemical reaction results in damage to abnormal cells or malignant tissue. Different types and intensities of light, as well as different photosensitizers, can lead to dramatically different outcomes for PDT.
This past year, scientists reviewed over a dozen clinical studies of PDT as a treatment for CIN. All of the studies included a clinical assessment of the CIN lesions’ response to PDT, and the complete response rate for PDT was up to 100% in some cases. A number of these studies also reported that PDT was very successful in eradicating the human papilloma virus, or HPV, a major cause of cervical cancer. The authors concluded that PDT is a safe and tolerable treatment for CIN, but further emphasized that more randomized clinical trials are needed to assess the true efficacy of this approach. This review was published in the June 2014 issue of Photodiagnosis and Photodynamic Therapy.
Treating CIN the Sensible, Photodynamic Way
The medical community has shown a strong interest in identifying non-surgical therapies in order to reduce the rate of progression from the low-grade CIN (also known as CIN 1, a minimally aggressive form) to the high-grade CIN, also referred to as CIN 2/3. In recent years, several clinical trials have indicated that PDT can produce in favorable response rates for patients with CIN.
For example, in a randomized placebo-controlled clinical trial at Hannover Medical School in Germany, the photodynamic approach led to a clearing of CIN lesions in twice as many patients when compared to the control group (57% versus 25%). These findings were reported in the August 2014 issue of Lasers in Surgery and Medicine.
Meanwhile, studies at the Third Military Medical University in Chongqing (Sichuan Province, China) have confirmed that binding the photosensitizer to folic acid (folate) can increase the agent’s ability to seek out and enter cervical cancer cells. Folic acid is a B vitamin better known for its ability to help lower the risk of developing cervical cancer. Based on findings from a series of laboratory experiments, the Chinese scientists propose that the folate-bound photosensitizer “has potential as an alternative treatment modality for cervical cancer,” as stated in the January 2015 issue of Oncology Reports.
A more recent report out of Hannover Medical School points to a very practical way to deliver effective PDT for CIN. This strategy utilizes a topical cream containing the well-studied agent, hexaminolevulinate (HAL). The photoactive cream is applied to the target tissue before exposure to light. Based on their review of the evidence, the Hannover researchers propose that “topical HAL PDT has potential as a non-surgical tissue-preserving treatment for CIN and persistent oncogenic human papilloma virus infections.”
The authors speculate that this practical approach to photodynamic treatment may eventually replace surgery in a large proportion of patients. “If the treatment is approved, it is very likely that physicians will want to use this treatment, as many patients will be keen to consider a non-surgical option,” the authors state in the February 2015 issue of Expert Opinion in Investigative Drugs.
Finally, researchers at National Taiwan University in Taiwan have been applying nanotechnology to the study of photosensitizers. They have found that different nano preparations can not only increase the amount of photosensitizer that becomes concentrated in the diseased tissue (or tumor), but also results in a higher quantum yield of reactive oxygen molecules for a stronger therapeutic effect. They contend that these “nanoagents” may provide a safe and easy photodynamic strategy for targeting cancer cells and destroying tumors while simultaneously minimizing side effects, as reported in the January 2015 issue of ACS Applied Materials Interfaces.
Why PDT Is Gaining Ground in Cancer Medicine
There are many reasons for PDT’s growing popularity among medical scientists interested in innovative treatment strategies that can circumvent the limitations of conventional treatment. To begin with PDT is relatively painless and minimally invasive. Treatments and can be completed in the clinic and then repeated many times without resulting in treatment resistance—a common problem with both chemotherapy and radiotherapy.
Speaking of those treatments, PDT also can be done in tandem with surgery, radiotherapy or chemotherapy. This ease of combining with other treatments makes PDT an especially promising and attractive treatment for malignant or premalignant diseases. PDT is also fairly portable and the treatment price is cheaper than most chemotherapy regimens.
Some research has shown that the degree of tumor eradication after PDT depends on a number of factors, such as the type of photosensitizer, medication dose, tumor type, and various aspects of the light dose and delivery. Some studies indicate that different ways of administering the photosensitizer can also change the treatment outcome, though this also depends on the particular disease situation.
In terms of cervical cancer, one of the main benefits of PDT is that little or no pain is experienced during the procedure, thus eliminating the need for anesthesia. Moreover, no bleeding occurs during or after PDT. In addition, PDT leaves the cervix intact and preserves fertility. No adverse effects of PDT on pregnancy or childbirth have been observed thus far.
The Promise of Bremachlorin-PDT
Recent laboratory studies of Bremachlorin® suggest that this photosensitizer can result in strong eradication of abnormal cells associated with CIN. This agent is known to have superior tolerability compared to other photoactive agents used in PDT. Whereas the first generation photosensitizers may result in mild pain and cramping, such effects have not been noted with the second- and third-generation photosensitizers such as Bremachlorin®.
Research out of Catholic University of Korea College of Medicine in Seoul (Korea) suggests that Bremachlorin® has many advantages over other photosensitizers and could play a substantial role in the treatment of cervical cancer as well. Their experimental data, originally published in the December 2004 issue of Cancer Research & Treatment, showed that light treatment of an HPV-associated tumor cell line (which can produce cervical cancer) in the presence of Bremachlorin® induced significant inhibition of the cancer cells.
Furthermore, Bremachlorin-PDT showed very strong inhibition of tumor growth. Further research is needed in order to better assess the treatment effects and the possibility of promoting long-term survival after a diagnosis of advanced cervical cancer. Ongoing investigations in the Netherlands have suggested that Bremachlorin-PDT may offer an optimal way to treat various kinds of cancer and precancer, though clinical trials are needed to test this assertion.
Support us by buying our book, The Medicine of Light, and ebooks from our Photoimmune Discoveries eBook Series.
Sources
Hillemanns P1, Einstein MH, Iversen OE. Topical hexaminolevulinate photodynamic therapy for the treatment of persistent human papilloma virus infections and cervical intraepithelial neoplasia. Expert Opin Investig Drugs. 2015 Feb;24(2):273-81.
Li PX, Mu JH, Xiao HL, Li DH. Antitumor effect of photodynamic therapy with a novel targeted photosensitizer on cervical carcinoma. Oncol Rep. 2015 Jan;33(1):125-32.
Tao XH1, Guan Y2, Shao D3, Xue W3, Ye FS3, Wang M3, He MH3. Efficacy and safety of photodynamic therapy for cervical intraepithelial neoplasia: A systemic review. Photodiagnosis Photodyn Ther. 2014 Jun;11(2):104-112.
Hillemanns P, Petry KU, Soergel P, Collinet P, Ardaens K, Gallwas J, Luyten A, Dannecker C. Efficacy and safety of hexaminolevulinate photodynamic therapy in patients with low-grade cervical intraepithelial neoplasia. Lasers Surg Med. 2014 Aug;46(6):456-61.
Yu J, Hsu CH, Huang CC, Chang PY. Development of therapeutic au-methylene blue nanoparticles for targeted photodynamic therapy of cervical cancer cells. ACS Appl Mater Interfaces. 2015 Jan 14;7(1):432-41.
© Copyright 2015, Photoimmune Discoveries, BV





 English
English Français
Français Deutsch
Deutsch Nederlands
Nederlands