Bile Duct Tumors: Testing Different Light-Based Strategies
Surgery is a potentially curative treatment for tumors found in the bile ducts, the ducts that carry bile from the liver and gall bladder to the intestines. The technical name for this unusual cancer is cholangiocarcinoma. Unfortunately, bile duct tumors (BDTs) often spread extensively along the ducts, well beyond the lesions that are observed at the time of diagnosis. This makes these tumors especially difficult to treat with surgery alone.
If cancer is found in the surgical margins (periphery of the surgical site), the prognosis is usually dismal. The conventional strategy in such situations is to use chemotherapy and radiation treatment to eliminate the residual cancer. To date, however, there is no evidence supporting the survival advantage of either radiotherapy or chemotherapy after surgery for these tumors.
On the other hand, in advanced inoperable BDTs, the placement of a metallic stent to help drain the bile can be a beneficial tactic. This strategy has been shown to improve the patient’s overall functioning and quality of life, although the treatment per se is not linked with any significant improvement in survival.
Stents are now a routine part of the treatment for bile duct tumors. A major problem with “stenting”, however, is that it has no impact on the disease itself. Thus, the tumor often continues to grow into the bile duct, eventually filling up and blocking the duct. This means that bile cannot flow through the duct. To help reverse this problem, physicians will often resort to the use of lasers or microwaves in an effort to unblock the duct.
Photodynamic therapy (PDT) has proved to be an effective way to improve treatment outcomes and prevent these problems from occurring in the first place. PDT can be understood as a more complex, sophisticated form of laser treatment. Since the 1980s, this light-based therapy has led to remarkable regressions of a wide range of malignant tumors, including those found in the bile duct.
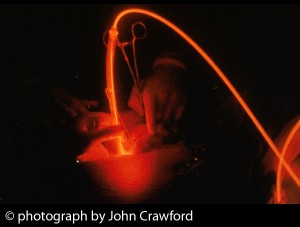
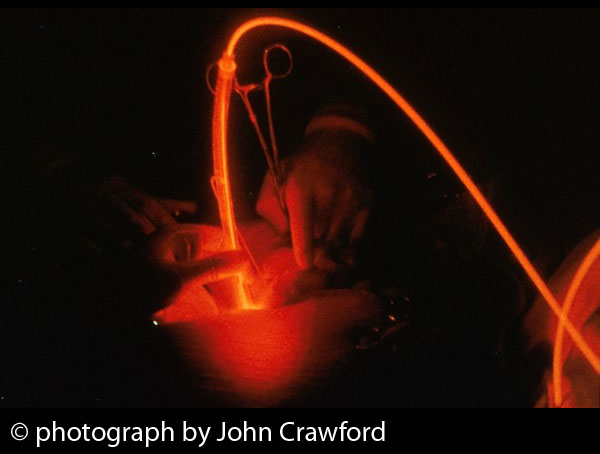
PDT entails the use of a light-sensitive medicine, called a photosensitizer or photosensitizing agent. This agent is activated by a specific type or wavelength of light. Upon being activated, the photosensitizer generates a form of oxygen that kills nearby cells. Oncologists well versed in the use of PDT will choose specific photosensitizers and wavelengths of light to treat different areas of the body with PDT.
With laser-based PDT, laser light is used to activate photosensitizing agents (photosensitizers) and trigger the destruction of cancer cells. PDT is now regarded as a technically feasible treatment for inoperable BDT. In randomized controlled trials, PDT has resulted in longer survival than stenting alone for patients diagnosed with this condition and for whom surgery was not an option.
One basis for the improved survival may be the powerful direct tumor-killing effect of PDT. A second basis may be the increased activity of the anti-cancer immune defenses. However, both of these factors depend heavily on the type of photosensitizer that is chosen for the light-based treatment.
Testing Different Photosensitizers
Research is now needed to test the survival advantages that result from PDT using different photosensitizers and laser treatments for patients with advanced bile duct tumors. Each photosensitizer has a unique capacity for responding to different wavelengths of light, and for entering living tissues, including those that comprise a tumor. The best photosensitizers are able to preferentially accumulate within the tumor, while being rapidly eliminated from normal tissues.
Testing different photosensitizers has emerged as a major focus of photodynamic research. Scientists at Nagasaki University Graduate School of Biomedical Sciences in Japan recently sought to evaluate two different photoactive agents. Half the group received Photofrin (generic name: porfimer sodium) while the other half received Laserphyrin® (talaporfin sodium).
This study found that the therapeutic effects of Laserphyrin-PDT were significantly stronger than those of Photofrin-PDT. Moreover, Laserphyrin-PDT had fewer side effects in terms of skin sensitivity to light (photosensitivity) following the treatment. Finally, the length of hospital stay was significantly decreased after Laserphyrin-PDT compared with Photofrin-PDT, as reported in the March 2014 Annals of Translational Medicine.
Combining PDT with Other Treatments
There is now sufficient evidence to conclude that PDT can play a key role in the treatment of patients with advanced bile duct tumors. Based on the findings from at least three clinical trials, we know that PDT together with stenting can significantly prolong survival compared to stenting alone. These studies found that the addition of PDT resulted in a three- to five-fold increase in survival for patients with inoperable tumors of the bile duct. Along with these survival improvements, these clinical studies indicated improvements in liver function, fewer treatment complications, and enhanced quality of life.
In view of these findings, many oncologists now concur that PDT with stenting is the treatment of choice for most patients with cholangiocarcinoma. Even when surgery is feasible, the tumor recurrence rate is very high, and long-term survival is rare. In particular, if there is any concern that the disease may have spread beyond the tumor margin, PDT will likely result in survival that is at least comparable to surgery.
The challenge is to determine the optimal PDT regimen for these patients, and also which combinations of conventional treatment will further enhance the overall effectiveness of photodynamic strategies. It is likely that the use of second-generation photosensitizers such as Bremachlorin® will further enhance treatment outcomes of PDT-based protocols, though of course clinical research will be needed to test this premise.
One of the factors that could improve the tumor-killing success of PDT is modulation of the cancer cell’s antioxidant system. Antioxidants are substances that protect the cell against free radicals, such as the highly reactive oxygen molecules that are generated by PDT. Finding ways to suppress the cancer cell’s antioxidant system could result in better treatment outcomes with PDT, as reported in the 18 September 2014 issue of Drug Design, Development and Therapy.
Support us by buying our book, The Medicine of Light, and ebooks from our Photoimmune Discoveries eBook Series.
Sources
Nanashima A, Isomoto H, Abo T, Nonaka T, Morisaki T, Arai J, Takagi K, Ohnita K, Shoji H, Urabe S, Senoo T, Murakami G, Nagayasu T. How to access photodynamic therapy for bile duct carcinoma. Ann Transl Med. 2014 Mar;2(3):23.
Patel J, Rizk N, Kedia P, Sharaiha RZ, Kahaleh M. Cholangioscopy-assisted photodynamic therapy for cholangiocarcinoma. Gastrointest Endosc. 2014 Dec 4. [Epub ahead of print]
Goenka MK, Goenka U. Palliation: Hilar cholangiocarcinoma. World J Hepatol. 2014 Aug 27;6(8):559-69.
Chen MH, Liang PC, Chang KC, Huang JY, Chang YT, Chang FY, Wong JM, Lin FH. Prototype of biliary drug-eluting stent with photodynamic and chemotherapy using electrospinning. Biomed Eng Online. 2014 Aug 19;13:118.
Lee HM, Chung CW, Kim CH, Kim do H, Kwak TW, Jeong YI, Kang DH. Defensive mechanism in cholangiocarcinoma cells against oxidative stress induced by chlorin e6-based photodynamic therapy. Drug Des Devel Ther. 2014 Sep 18;8:1451-62.
© Copyright 2014, Photoimmune Discoveries, BV


 English
English Français
Français Deutsch
Deutsch Nederlands
Nederlands