New Light on Persistent Candida Yeast Infections
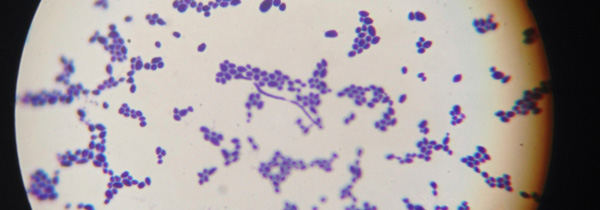
Photograph of Candida albicans under a microscope.
It has been estimated that three out of four women will experience a yeast infection at some point in their lives. Most of these are vaginal infections with the Candida yeast (or fungus), and they often result in intense itching, swelling, and irritation. Though these infections, also known as candidiasis, can be spread by sexual contact, candidiasis is generally not regarded as a sexually transmitted condition. The growth of Candida yeast is kept in check by the beneficial bacteria known as lactobacillus as well as other organisms that naturally inhabit the gut and vaginal tissues.
If there’s an imbalance in the bacterial populations—perhaps due to antibiotics, stress, weakened immunity, or excess sugar in the diet—this can lead to an overgrowth of yeast, resulting in the aforementioned symptoms of vaginal yeast infections. Many women have recurring yeast infections and problems getting rid of a yeast infection with conventional treatment.
To make matters worse, Candida displays an uncanny ability to acquire resistance to antifungal drugs, posing a major obstacle to successful treatment. One fundamental cause of this treatment resistance is a protective coating, or biofilm, which also enables development of invasive fungal infections.
Few antifungal treatments have been effective against fungal biofilms, and this fact has further accelerated the search for alternatives to antifungal drugs. The light-based approach known as photodynamic therapy (PDT) involves the use of light-sensitive compounds (photosensitizers) in combination with harmless visible light of the correct wavelength.
These photosensitizers tend to become concentrated within abnormal cells, such as Candida and other fungal organisms. In the presence of oxygen, the photosensitizer then transfers energy or electrons to molecular oxygen, generating reactive oxygen species that can destroy the Candida and other disease-causing microbes.
An International Survey of Recent Studies
Researchers at the Center for Lasers and Applications in São Paulo, Brazil, recently investigated the effects of PDT on Candida infection and inflammatory cells in an animal study of vaginal candidiasis. Female mice were inoculated with Candida and then separated into different treatment and control groups.
The study demonstrated that PDT with the photosensitizer methylene blue, and red laser treatment, is a promising therapy for vaginal candidiasis. This treatment was very successful in curbing fungal infections as well as reducing biofilm and inflammatory signals associated with the vaginal infection, as reported online ahead-of-print in the 1 May 2014 issue of Photodiagnosis and Photodynamic Therapy.
Another recent study was conducted at King Saud University’s College of Applied Medical Sciences in Riyadh, Saudi Arabia. In this review of the evidence, a total of 15 studies (3 clinical and 12 experimental) were found to have reported PDT as an effective antifungal treatment strategy.
The reseaerchers concluded that the “clinical effectiveness of antimicrobial PDT as a potent therapeutic strategy for oral fungal infections requires further investigations,” as reported in the May 2014 issue of Photochemical & Photobiological Sciences. PDT could soon prove to be the logical alternative to conventional treatment methods when Candida infections keep recurring or respond poorly to the standard pharmacetical approach.
Finally, a study at Columbia University Medical Center in New York City (USA) focused on the different types of Candida albicans based on features of the yeast’s cell walls, as the effectiveness of PDT may depend in part on the cell wall structure of microorganisms. Two basic types of cell wall were identified, serotype A and serotype B.
The researchers compared the sensitivity of biofilms of C. albicans serotypes A and B to PDT. They found that the photosensitizer alone (without light) had no effect on the biofilms. With the application of laser light, however, there was a significant destructive effect only on the serotype B cells, suggesting that PDT may only be able to limit the growth of certain Candida organisms, as reported online ahead-of-print in the 12 April 2014 issue of Lasers in Medical Science.
Support us by buying our book, The Medicine of Light, and ebooks from our Photoimmune Discoveries eBook Series.
Sources
Machado-de-Sena RM1, Corrêa L2, Kato IT3, Prates RA4, Senna AM5, Santos CC3, Picanço DA3, Ribeiro MS6. Photodynamic therapy has antifungal effect and reduces inflammatory signals in Candida albicans-induced murine vaginitis. Photodiagnosis Photodyn Ther. 2014 May 1.
Javed F1, Samaranayake LP, Romanos GE. Treatment of oral fungal infections using antimicrobial photodynamic therapy: a systematic review of currently available evidence. Photochem Photobiol Sci. 2014 May;13(5):726-34.
Rossoni RD1, Barbosa JO, de Oliveira FE, de Oliveira LD, Jorge AO, Junqueira JC. Biofilms of Candida albicans serotypes A and B differ in their sensitivity to photodynamic therapy. Lasers Med Sci. 2014 Apr 12.
© Copyright 2014, Photoimmune Discoveries, BV

 English
English Français
Français Deutsch
Deutsch Nederlands
Nederlands